Ramin Rak is a board-certified neurosurgeon with years of experience specializing in complex tumors, spine treatments, awake craniotomies, and skull base surgeries.
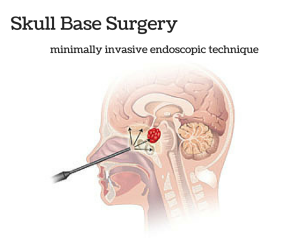
Skull base surgery is a specialized type of surgery performed to treat tumors and other diseases occurring in certain areas of the skull such as behind the eyes or in the nasal cavity. The skull is made up of bones and cartilage, forming the face and the cranium. The bones that form the base of the cranium also form the eye socket, some of the sinuses, the roof of the nasal cavity, as well as the bones surrounding the inner ear. The base of the skull is a very complex area where many vital parts of the body pass through including blood vessels, nerves, and the spinal cord.
Skull Base Surgery requires a multidisciplinary approach often involving ear, nose, and throat surgeons, neurosurgeons, plastic surgeons, radiologists, pathologists, oncologists, and other specialists. There are two main ways to perform skull base surgery. It may be done through a minimally invasive endoscopic procedure. This involves making a small incision through the natural openings of the skull, normally the nose or mouth. A small hole may also be made just above the eyebrow. Through this method, a neurosurgeon is able to remove the growth through a thin lighted tube referred to as an endoscope. An MRI picture of the skull base will usually be taken during this process to ensure that the entire growth has been removed successfully. The second way to perform skull base surgery is often referred to as traditional or open skull base surgery. This procedure requires making an opening in the skull. Parts of bone may be removed in order to reach the growth and have it properly removed.
Listed below are some of the common growths and conditions that may be treated with skull base surgery:
- Growths caused by infections
- Pituitary tumors
- Sinus tumors
- Glomus tumors
- Cysts developed from birth
- Cerebrospinal fluid leak
- Meningiomas
- Chordomas
- Trigeminal neuralgia
- Acoustic neuroma