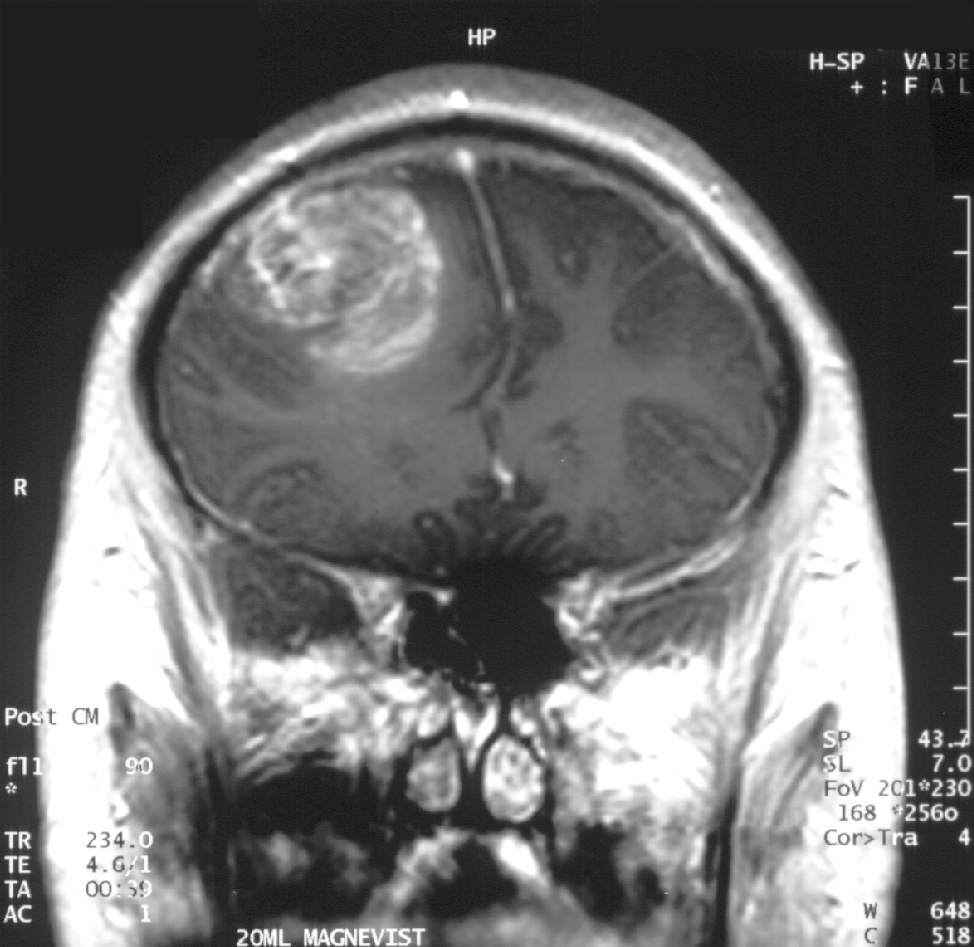
Ramin Rak practices his advanced knowledge of microneurosurgical techniques at Neurological Surgery P.C. on Long Island.
Here, he specializes in awake craniotomies, spinal surgeries, skull-based surgeries, and treatment of tumors.
More information on these complex procedures can be accessed through his Pinterest page.
A stroke is caused by a disturbance in the blood supply and results in the loss of function.
An ischemic stroke is caused by a clot that obstructs blood flow, while a hemorrhagic stroke is a result of a rupturing blood vessel. A transient ischemic attack can also occur, which is essentially a mini stroke caused by a temporary clot. Both types of strokes are extremely serious, as they are the number four cause of death, and the leading cause of adult disability in the United States.
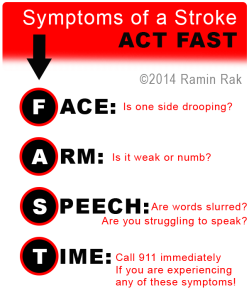
According to strokeassociation.org, F.A.S.T is an easy way to remember the sudden signs of a stroke:
- Face Drooping- If one side of your face is drooping or your smile is uneven, it could indicate a stroke.
- Arm Weakness- When one arm is weak, numb, or drifts downward when your arms are raised, seek immediate medical attention.
- Speech Difficulty- If someone is struggling to form words or unable to repeat a simple sentence, a stroke may be the cause.
- Time to call 911- If you are experiencing any of these symptoms, call 911 immediately, even if the symptoms go away.
Beyond these core symptoms, a person may also present numbness of the leg, arm or face; trouble seeing; an unexplained sudden, severe headache; dizziness or loss of coordination; and confusion or trouble understanding.
Quick stroke treatment can save lives, so it is crucial to seek immediate medical attention if you have shown any of the above symptoms. After a doctor makes a diagnosis, they will begin a treatment plan specific to the cause of the stroke.