Thank you for visiting my blog. My name is Dr. Ramin Rak and I am a surgeon with Neurological Surgery, P.C.
I specialize in treating complex spinal and brain complications at the eleven different medical facilities affiliated with Neurological Surgery, P.C. and I am a member of the organization’s Neurosurgeon Brain Tumor Team.
The Brain Tumor team includes an Endovascular Neuroradiologist, two Neuro-oncologists, a Neuropsychologist, myself, and seven other neurosurgeons:
- Dr. Michael H. Brisman, M.D., F.A.C.S.
- Dr. Jeffrey A. Brown, M.D., F.A.C.S.
- Dr. Lee Eric Tessler, M.D., F.A.A.N.S.
- Dr. Alan Mechanic, M.D., F.A.C.S.
- Dr. Robert N. Holtzman, M.D.
- Dr. Vladimir Dadashev, M.D.
- Dr. Gerald M. Zupruk, M.D., F.A.A.N.S.
The rest of the Brain Tumor Team and I work to treat brain tumors and complications caused by tumors, including gioblastoma, medulloblastoma, acoustic neuroma, and schwannoma.
Schwannoma is a homogenous tumor that is made up entirely of Schwann cells, which conduct nervous impulses along axons, provide trophic support for neurons, and support nerve development and regeneration.
The tumor cells are always on the exterior of the nerve though the tumor itself can cause nerve damage by pushing the nerve aside or into bone. Schwannomas become malignant in less than 1% of cases and are slow growing, but should still be treated if weakness numbness, pain or other symptoms are seen.
The Brain Tumor Team at NSPC uses surgery or stereotactic radiosurgery to treat schwannomas with radiosurgery being an option when the tumor is located in the head or spine.
The most common treatment is stereotactic radiosurgery, or the use of a machine called the Gamma Knife to focus high-powered x-rays at the spot of the tumor. Between 80 and 90% of the patients who opt instead to have surgery report that pain, weakness, and numbness disappears following the procedure.
Learn more about how the Brain Tumor Team treats schwannomas here.
Thank you for reading,

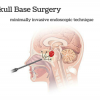
This is an example of a schwannoma. It typically has dense areas called Antoni A (black arrow) and looser areas called Antoni B (blue arrows). The cells are elongated (spindle shaped) and the nuclei have a tendency to line up as you see here in the Antoni A area. (via ucsf.edu)