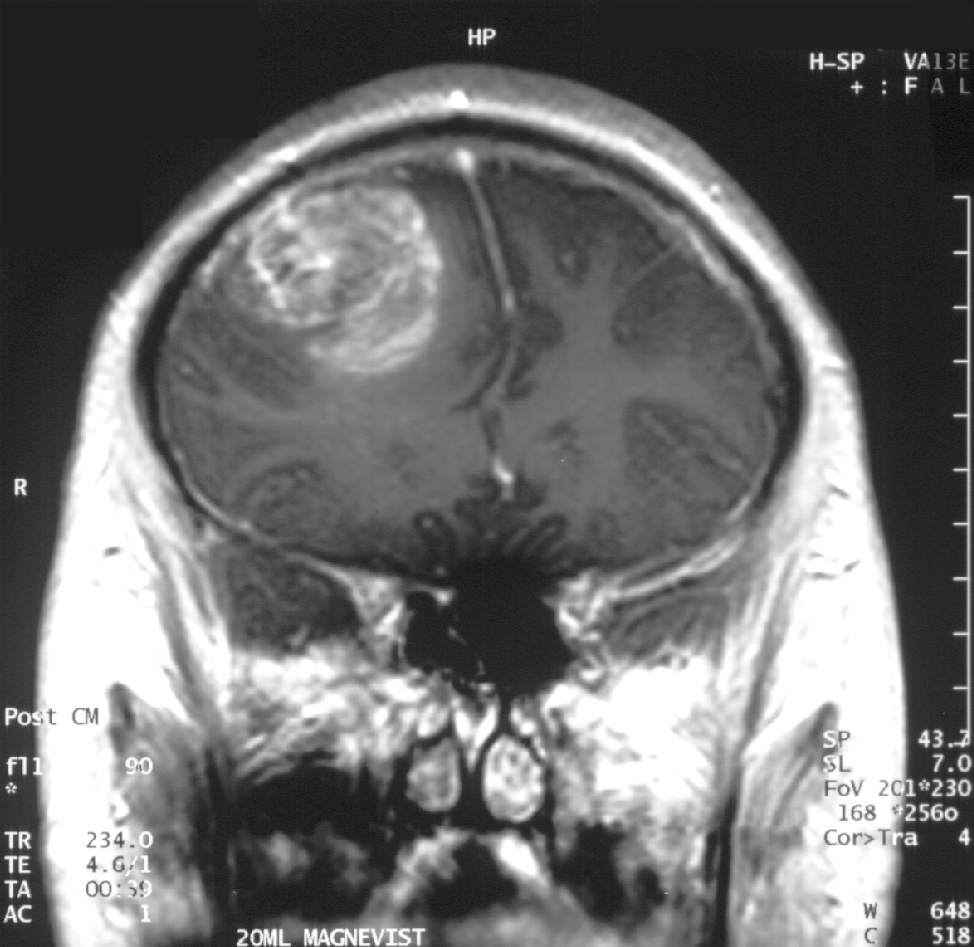
Glioblastoma in an x-ray. (Source: Wikipedia.org)
Hello again, this is Ramin Rak, back with another post about a medical procedure I performed at Neurological Surgery, P.C. in Long Island.
I specialize in treating disorders related to the brain and spine, and recently removed a glioblastoma multiforme tumor during a high-profile surgery.
Glioblastomas (GBM) are tumors found in the cerebral hemisphere or spinal cord.
These tumors are highly cancerous due to their ability to reproduce cells quickly. In addition, they are supported by a large network of blood vessels. The cause of these tumors are unknown but due to their rapid growth, symptoms commonly involve pressure on the brain. Headache, vomiting, nausea, and drowsiness are the most common. Treating GBM is very difficult because these tumors contain many different types of cells. Furthermore, the network of tentacles in the brain make it extremely difficult to remove these tumors without affecting the patient’s language and coordination. For these reasons, your surgeon may decide to combine several approaches to treat your GBM.
Recently, Donald Squire, 52, of East Northport was diagnosed with a GBM that required surgery.
His only symptom was a twitching in one of his eyes. His wife suspected a stroke but brain scans revealed that the twitching was due to a tumor. Fortunately, I was able to use proprietary technology to enter the inner labyrinths of his brain and remove the tumor. To reach the tumor, I used brain-mapping technology and neuronavigation, which made it possible to move eloquently throughout the delicate areas of his brain. The patient was awake during surgery in order for me to monitor his language, vision, and speech. After the surgery, I had concerns that Squire might lose some of his peripheral vision, but he hasn’t noticed any changes. Squire is very fortunate to have had access to this technology, as not too long ago, this area of his brain would have been unreachable using conventional techniques.
You can learn more about Squire’s procedure here: http://grow-your-practice.net/wp-content/uploads/2013/07/Dr-Rak-Newsday-062213.pdf
Thanks for reading,
Ramin Rak
You can learn more about me and my specialties in the Commack Patch, or by connecting with me on Doctor’s Hangout: www.doctorshangout.com/profile/DrRaminRakMD