Hi all, Ramin Rak here with another blog post about a complicated neurosurgical procedure I perform at Neurological Surgery, P.C.: aneurysm coiling.
I primarily treat conditions in the brain and spine so I only perform aneurysm coiling to address brain aneurysms. Endovascular aneurysm coiling is one of two techniques (along with open surgical clipping) that can be used to treat brain aneurysms, but sometimes a physician will choose to closely observe an aneurysm instead of recommending one of these two treatments.
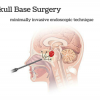
Aneurysm coiling is a minimally invasive endovascular procedure performed to treat an aneurysm, which is a balloon-like bulge of an artery wall (learn more).
As an aneurysm grows, it will thin and weaken until it becomes so thin that it leaks or ruptures. A ruptured aneurysm will release blood into the space around the brain, called a subarachnoid hemorrhage, and is life threatening. Treatment involves stopping blood from flowing into the aneurysm but still allowing blood to flow freely through the normal arteries. While open surgical clipping accomplishes this from the outside, aneurysm coiling does so from the inside.
I begin the procedure by giving the patient anesthesia while they are on the x-ray table.
Next, I locate the femoral artery and use a needle to insert a long plastic tube (the catheter) into the bloodstream. Dye is then injected through the catheter to make blood vessels visible on my x-ray monitor, allowing me to guide the catheter to one of four arteries in the neck that lead to the brain. After the catheter is placed, I take x-ray photos and use them to take measurements of the aneurysm.
A second smaller catheter travels through the first catheter and makes its way to the aneurysm itself.
Small platinum coils are then passed through the catheter until they emerge in the aneurysm, and this process continues until the aneurysm is completely packed with coils. I then inject contrast agent so that I can confirm that blood is no longer flowing into the aneurysm and finally close the puncture site in the artery.
Endovascular aneurysm coiling has a long-term success rate between 80 and 85%.
Thanks for reading,
Ramin Rak
Learn more about my specialized neurosurgical procedures on Brand Yourself: http://raminrak.brandyourself.com/ or visit my WordPress blog.