Ramin Rak
Dr. Ramin Rak, M.D Neurosurgeon
About

Board-certified surgeon Ramin Rak, M.D., F.A.A.N.S., F.A.C.S, is an expert with vast experience in micro-neurosurgical techniques. He uses his expertise in these techniques to perform complex and spine surgeries and has even published several dozen articles and book chapters in neurosurgical journals and book atlases. Dr. Ramin Rak is able to perform a number of complex neurological and spine surgeries but he specializes in complex spine treatments, tumors, skull-based surgeries, and awake craniotomies. In fact he has even used his expertise to establish awake craniotomy programs at numerous Long Island hospitals. Dr. Ramin Rak began his medical studies in Belgium, by earning undergraduate degree with high honors in Medical Basic Sciences, and then his medical degree from the Free University of Brussels. He then gained hands-on training in Washington, DC, completing an externship and then an internship in the Washington Hospital Center’s Department of Surgery. Next, he served as a … Read More
Education & Training

Board certified neurosurgeon Dr. Ramin Rak is very respected within his field. He specializes in performing awake craniotomies, skull-based surgeries, complex spine surgeries, and treatment of tumors at Neurological Surgery P.C. using his advanced knowledge of micro-neurosurgical techniques. He is able to complete this work thanks to his education and training with some of the best neurosurgical professionals in the world. Before a neurosurgeon can practice in the United States, he or she is … Read More
Awake Craniotomies
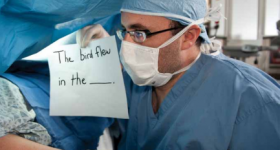
Dr. Ramin Rak has received glowing reviews from former patients thanks to his superb bedside manner, and he is able to demonstrate this bedside manner while performing awake craniotomies at Neurological Surgery P.C.. Awake craniotomies are necessary when a tumor is located in one of the eloquent cortices intertwined with the tissue. For tumors that are this hard to get to, there is a greater risk to the patient’s motor, sensory, and linguistic abilities. Surgeons need to monitor these … Read More
Micro-Neurosurgery

Ramin Rak specializes in micro-neurosurgical techniques, a form of neurosurgery that requires an operating microscope. This expertise in micro-neurosurgery allows him to clearly target structures and the surrounding normal anatomy. Ramin Rak uses a counter-balanced operating microscope that has a digital video camera connecting to it. This camera will connect to monitors in order to ensure coordination between the doctor and his surgical team. Ramin Rak tries to make each and every … Read More
© Copyright 2013 Dr. Ramin Rak, MD · All Rights Reserved · · Google+ ·Admin

Connect with me